-Acute Pharyngitis-
-Acute pharyngitis is one of the most common conditions encountered in the office practice
-Group A Streptococcus (GAS) makes up about 5-15 percent of the adults presenting with pharyngitis
-Etiologies include GAS, mononucleosis, CMV, HSV, and many other viruses including influenza
-Non Group A Streptococcus a groups C and G cause pharyngitis but do not cause rheumatic fever
-Diphtheria, Neisseria Gonorrheae, Chlamydia, Mycoplasma, and Tularemia can cause also
-Symptoms include sore throat, worse with swallowing, headache, malaise, and anterior neck pain form lymphadenopathy
-Exam may reveal pharyngeal erythema, tonsillar hypertrophy, and purulent exudates. Palate petechiae may be present with lymphadenopathy
-may have hepatosplenomegaly with mono
-Centor Criteria-tonsilar exudate, tender anterior cervical lymphadenopathy, fever, and absence of cough
-The presence of 3 or more Centor Criteria a rapid antigen detection test should be performed (Rapid Strep)
-If there is two or less of the Centor Criteria neither throat culture or rapid strep is necessary
-Other dangerous infections causing sore throat include epiglottis, peri-tonsilar abscess, submandibular space infection, retropharyngeal space infections and primary HIV
-Best to use tylenol or NSAIDS for systemic pain control
-Can use topical lozenges or sprays
-Use of glucocorticoids is controversial
-Penicillin VK, Amoxicillin or Bicllin CR times one dose treatment of choice
-Can use cephalosporins or macrolides for alternative therapy
-Augmentin for beta lactam resistance
-Aphthous Ulcers-
-aphthous ulcers are also known as canker sores
-they are painful lesions that appear as localized, shallow, round, ulcers with a grayish base
-local cell mediated immunity may be important in pathogenesis
-factors that predispose include trauma, hormonal factors, drug sensitivity, food sensitivity, immunodeficiency, and emotional stress
-also seen in patients with celiac disease or inflammatory bowel disease
-Vitamin and mineral deficiency have been implicated in the pathogenesis
-Treatment includes topical steroids and topical analgesics (magic mouth wash)
-Diseases of the Teeth and Gums-
-Periodontal disease is disease that effect the gingiva, cementum, periodontal ligament and the alveolar bone
-Periodontitis is inflammation of the gingiva and the alveolar bone
-Gingivitis dose not affect the alveolar bone. It is characterized by inflammation land gingival redness and swelling. Bleeds easy
-Gingivitis can be provoked by drug or pregnancy.
-Scurvy is a gingival disease provoked by Vitamin C Deficiency
-Necrotizing ulcerative gingivitis is called trench mouth. It can cause systemic symptoms, pain, ulcerative necrotic gingiva. It is associated immune disorders and malnutrition
-Dental infections can cause hematogenous disseminations of the infection and cause to seed native or prosthetic heart valves, joints or other devices
-Dry socket is osteomyelitis of the alveolar bone that can happen after dental extractions
-Dental caries come as a complication of dental decay. Treated with filling restoration and prevention
-Pulpitis is inflammation of dental pulp from dental decay presents with severe dental pain and temperature sensitivity
-Antibiotics help with local spread of infection and prevent hematogenous dissemination.
-It is also recommended for patients with prosthetic heart valves and artificial devices that get antibiotic prophylaxis prior to any procedure
-Usually penicillin VK is recommended or clindamycin
-Epiglottitis-
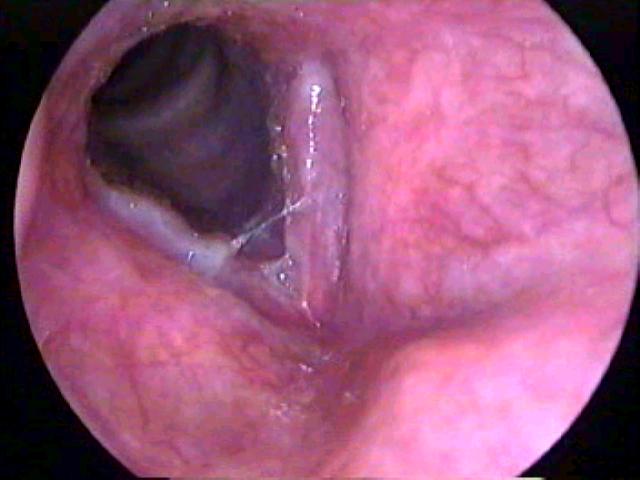
-Epiglottis is inflammation of the epiglottis and adjacent supraglottic structures
-Can lead to life threatening airway obstruction
-It results from direct spread of the epithelial layer of the bacteria
-Most common cause is Haemophilus Influenzae type B (HIB)
-Can be caused by many other bacteria or even viruses less likely
-The incidence of epiglottis has decreased with the HIB vaccine
-can come from noninfectious causes such as trauma, thermal injury or foreign body ingestion
-can come from fungal causes especially in immunocomprimised hosts
-presents with an abrupt onset of dysphagia, drooling, and respiratory distress. Also see fever and sore throat
-direct visualization confirms the diagnosis
-on soft tissue neck should see "thumb sign"
-should try to minimize agitation for exam if high index of suspicion. Have patient intubated in the OR with anesthesia
-Airway maintenance is the most important feature in the treatment of Epiglottis
-Intubation for 2-3 days is usually necessary before the patient can be safely extubated
-the role of glucocorticoids are controversial
-Empiric antibiotic therapy should include ceftriaxone and an anti-staph agent clindamycin or vancomycin
-racemic epinephrine may provide some temporary relief
-Laryngitis-
-Acute laryngitis is a self limited inflammatory condition lasting less than 3 weeks usually associated with a upper respiratory infection or voice strain
-The etiology is usually viral with acute laryngitis
-Strep Pneumonia, H. Influenzae, and M. Catarrhalis have been isolated in patients with acute laryngitis
-Acute laryngitis from a URI usually has sore throat, hoarse voice, and runny nose.
-Chronic laryngitis it typically associated with one or more chronic irritants, that cause inflammation
-Oral Candidiasis-
-Also known as thrush
-It is a common infection in infants. It occurs in adults who wear dentures, treated with antibiotics, radiation therapy, or chemotherapy
-Oral candidia also is seen in those in immunodeficient stats such as HIV
-Can occur with patients taking oral glucocorticoids
-Usual pathogen is candidia alblicans
-Pseudomembrane type or oral candidia is most common and is white plaques on buccal mucosa, palate, and tongue
-The other form is atrophic form also known as denture stomatitis. Cotton mouth, loss of taste, and pain with eating
-Treatment involves nystatin swish and spit for uncomplicated oral thrush
-Oral Herpes Simplex-
-the herpes simplex virus is spread by direct contact with the epidermis and eventually the sensory and autonomic nerve endings
-the lesions are painful and can last for 10-14 days
-the lesions present as grouped vesicles on an erythematous base
-these are also known as cold sores
-treatment is Acyclovir 200 mg PO five times a day or 400 mg TID
-you can also use Famciclovir 500 mg TID or Valacyclovir 1000 mg BID
-Oral Leukoplakia-
-Oral leukoplakia is a precancerous lesion that is white patches or plaques of the oral mucosa
-It is hyperplasia of squamous epithelium
-It is associated with human papilloma virus (HPV)
-One to twenty percent of these lesions will progress to carcinoma within 10 years
-Smokeless tobacco is a major risk factor
-Oral hairy leukoplakia occurs in HIV patients is not premalignant. It is caused by the Epstein Barr Virus
-These lesions need biopsied and monitored frequently
-Peritonsillar Abscess-
-Peritonsillar Abscess is a collection of pus between the capsule of the palatine tonsil and the pharyngeal muscles
-Peritonsillar infection is preceded by tonsillitis and progresses to cellulitis to phlegmon to abscess.
-It can also occur without preceding infection
-Peritonsillar abscess can compromise the upper airway and surrounding structures
-Peritonsillar abscess usually present with sore throat, fever, and a hot potato voice. Pooling of saliva or drooling may be present.
-Trismus may be present
-If there is these is a concern of possible epiglottis or the diagnosis of peritonsillar abscess is not definitive, imaging of the neck must be accomplished. CT scan with IV contrast of soft tissue neck
-Empiric antibiotics for Group A Strep and Staph aureus and respiratory anaerobes should be accomplished
-Unasyn or Clindamycin is appropriate antibiotic coverage
-If there is no response to therapy or there is airway issues vancomycin should be used also in addition to above antibiotics
-Ultimate treatment for peritonsillar abscess is incision and drainage
-Parotitis-
-Bacterial Parotitis is usually caused by Staph Aureus and mixed oral aerobes and anaerobes
-Can occur in the presences of dehydration and poor oral hygiene
-May occur from salivary stasis and retrograde seeding of the Stensen's Duct of the parotid gland with oral flora
-Stensen's duct may also be obstructed with a salivary stone or tumor
-On physical exam it presents as a sudden onset of firm erythematous swelling of the pre and posterior auricular area that extends to the angle of the mandible
-Staphylococcus aureus is the most isolate bacteria
-Imaging studies such as CT scan of soft tissue neck with IV contrast or Ultrasound is helpful to determine if abscess or stone is present
-Treatment is with IV antibiotics. Naficillin and Metronidazole recommended for immunocompetent patients.
-If patient is immunocompromised, vancomycin plus cefepime or imipenem is recommended
-Silaadenitis-
-typically presents with pain, swelling and erythema in the area of the gland
-there may be pus draining from the affected duct
-may be caused by salivary duct stone
-usually resolves within 7-10 days when treated with antibiotics
-if does not improve may develop an abscess and need to do a CT scan with IV contrast of the soft tissue neck
-dicloxacillin or cephalexin is ideal treatment for staph coverage
-Benign and Malignant Neoplasms of Oral Cavity-
-Squamous Cell Carcinoma of the mouth is associated with ulcers or masses that do not heal with dental changes or poorly fitted dentures
-Tongue and lip cancers present as ulcerative lesions usually painful
-Persistent plaques, ulcers, or erosions should be biopsied
-Melanoma-should be considered on oral pigmented lesions that have irregular borders and asymmetry or increasing diameter. Surgery is treatment of choice
-Amalgam Tattoos-are blue black macules seen in the gingiva near dental fillings. Benign lesions.
-Fordyce Spots-benign tumors of sebaceous gland etiology. These are isolated white to yellow papules prominent on the vermillion and mucosal border
-Mucoceles-fluid filled cavities with mucous glands lining of the epithelium. These are typically seen after mild oral trauma or disruption of the salivary duct. Rupture can lead to complete resolution.










No comments:
Post a Comment